|
Case Report
Vertebrobasilar dolichoectasia: A rare presentation to the otolaryngologist
1 Core Surgical Trainee, Stockport NHS Foundation Trust, Stockport, United Kingdom
Address correspondence to:
Jessica Daniels
MBChB, MRes, Core Surgical Trainee, Stockport NHS Foundation Trust, Stockport,
United Kingdom
Message to Corresponding Author
Article ID: 100001Z18JD2020
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Daniels J, Rudic M. Vertebrobasilar dolichoectasia: A rare presentation to the otolaryngologist. J Case Rep Images Otolaryngol 2020;1:100001Z18JD2020.ABSTRACT
Introduction: Vertebrobasilar dolichoectasia (VBD) is a pathological process causing elongation, tortuosity, and dilation of blood vessels. When intracranial vessels are affected they can exert pressure on surrounding structures.
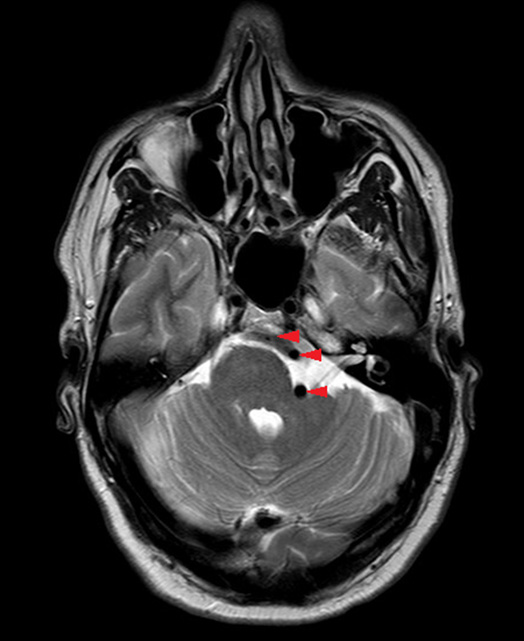
Case Report: A 50-year-old man presented with a six month history of left sided continuous, high pitched tinnitus, and hearing loss. A magnetic resonance imaging (MRI) scan revealed VBD causing deformation of the vestibulocochlear nerve and brain stem at the pontomedullary junction. The decision was taken not to intervene for two reasons; the symptoms were not affecting the patient′s quality of life, second, the vertebral artery was not abutting the vestibulocochlear nerve. He was managed conservatively and referred to the stroke team.
Conclusion: Vertebrobasilar dolichoectasia can present with multiple or isolated cranial neuropathies. As a rare cause of vestibulocochlear symptoms, VBD should be considered if symptoms cannot be explained. Vertebrobasilar dolichoectasia carries an increased risk of death from ischemic stroke, hemorrhagic stroke, and brain stem compression. Evidence-based treatments are lacking and there is no consensus on the optimal management. Randomized control trials are needed urgently to improve outcomes in this patient group.
Keywords: Ischemic stroke, Vertebrobasilar dolichoectasia, Vestibulocochlear neuropathy
Introduction
Tinnitus is an extremely common symptom that has the potential to impact sleep, mental health, and quality of life [1]. It currently affects 6 million people in the UK, 10% of the population [2]. It is widely accepted that MRI of the internal auditory meatuses (IAMs) should be considered for patients presenting to the otolaryngology clinic with unilateral tinnitus to rule out retrocochlear pathology [3]. While the most common cause of tinnitus is idiopathic, rarely it can be caused by more sinister pathology. A very rare but important cause of unilateral tinnitus is distortion of the eighth cranial nerve by an aberrant blood vessel [4],[5]. Vertebrobasilar dolichoectasia is the elongation, dilation, and tortuosity of the vertebral and basilar arteries. While this condition is uncommon, it carries a significant risk of morbidity and death from ischemic stroke, hemorrhagic stroke, and brain stem compression [6],[7] Its diagnosis is clinically important to monitor the progression of the arterial changes, manage modifiable risk factors for ischemic stroke including hypertension and for consideration of antiplatelet therapy [7] .
Vertebrobasilar dolichoectasia may present with cerebrovascular events or compressive symptoms. The vertebral arteries are in close proximity to the cerebellopontine angle (CPA), thus VBD can cause compression and deformation of the cranial nerves exiting in the brain stem at this location [5],[7]. Commonly the trigeminal, facial, and vestibulocochlear nerves are affected, thus VBD can present as an isolated cranial neuropathy or with a multitude of neurological symptoms making its diagnosis clinically challenging.
A number of acquired and genetic risk factors have been identified for the development of VBD. Acquired factors include increased age, hypertension, tobacco smoking, and increased alcohol consumption; notably, all are cardiovascular risk factors [5]. Male sex, family history of cerebrovascular disease, and connective tissue disorders including Marfan’s disease, Elher–Danlos syndrome, and Fabry’s disease are known nonmodifiable risk factors for the condition [5].
Here, we present a rare case of VBD in association with unilateral tinnitus and hearing loss in a patient with no risk factors for the condition.
Case Report
A 50-year-old gentleman presented with a six month history of left sided, high pitched, continuous, nonpulsatile tinnitus with mild left sided hearing loss. He did not complain of any other otogenic symptoms and his past medical history was unremarkable. Otoscopy and cranial nerve examination were normal. His audiogram showed left high frequency sensorineural hearing loss with an average hearing threshold of 40 dB (Figure 1). An MRI IAM was organized that revealed VBD causing significant distortion and deviation of the left VI, VII, and VIII nerve complex at the level of the pontomedullary junction as well as localized mass effect and displacement of the brain stem (Figure 2). The case was discussed at the skull base multidisciplinary team meeting. Surgical intervention was not advised as the vertebral artery was not in direct contact with VIIIth nerve. As the patient’s quality of life was unaffected by his symptoms, the risks of surgery were outweighed by the benefits. No intervention was made and the patient was discharged as per their request. The patient’s general practitioner (GP) was advised to review and manage modifiable risk factors for ischemic stroke and refer to the stroke team for consideration of antiplatelet therapy.
Discussion
Vertebrobasilar dolichoectasia is a progressive pathological process affecting arteries around the CPA, an area particularly vulnerable to compression and distortion due to the limited space in the posterior fossa. Deformation of the brain stem can present with varied symptoms including no symptoms, progressive neurological impairment, and/or death [5],[7]. The exact etiology of VBD is still unknown and both acquired and congenital factors may contribute to its development [7]. Aberrant vascular remodeling due to increased vessel wall sheer stress triggers a biochemical cascade. Subsequently causing weakening of the vessel wall resulting in dilation, elongation, and tortuosity [5]. These arterial changes result in morbidity and mortality by three mechanisms; thromboembolism causing stroke, arterial rupture causing subarachnoid hemorrhage, and brain stem compression [7]. Therefore, suggested treatments aim to prevent these complications occurring [7].
Vertebrobasilar dolichoectasia is well reported as a cause for vestibulocochlear symptoms, the facial and trigeminal nerves are also frequently affected by compression [5],[8]. While our patient did show physical deviation of the V, VII, and VIIIth nerve complex and did not demonstrate any associated neuropathy of V or VIIth cranial nerves. This raises some doubt as to whether VBD was the sole causative factor for the hearing loss and tinnitus in this patient, but no other cause was identified. A previous study found that only 47% of patients with vestibulocochlear symptoms and VBD confirmed on imaging could categorically attribute their symptoms to peripheral nerve compression. They concluded that the vestibulocochlear manifestation was due to central impairment including cerebellar dysfunction secondary to compression [8]. A recent report of four cases discussed a patient with a similar presentation to this case; left side dominant tinnitus and high frequency hearing loss with left sided VBD causing significant deviation of the VIIIth nerve root and likely microvascular compression [9]. They postulate that the difficultly in diagnosis is that correspondence between the compression site and symptoms may not be obvious.
The prevalence of VBD in the general population is unknown [5]. The uncertainty has been attributed to referral patterns and a lack of standardized diagnostic criteria until 1986. Vertebrobasilar dolichoectasia is however known to be most prevalent in patients affected by ischemic stroke, its prevalence in this population is quoted at 12% [7],[10]. It is known that VBD is an independent risk factor for stroke, most commonly affecting the posterior circulation [11],[12]. In a systematic review the five year risk of transient ischemic attack was 10.1% and the five year risk of ischemic stroke was quoted at 17.6%. The five year risk of intracranial hemorrhage was lower at 4.7% [6]. In comparison, the combined lifetime risk of ischemic and hemorrhagic stroke in patients aged 50 years is <1% [13].
The risk of stroke can be reduced by surgical and endovascular procedures with varied results. Given that VBD progresses overtime with increasing vessel dilation, it has been postulated that reducing the blood pressure in the vessel will prevent disease progression [14]. This can be achieved by a microsurgical approach by changing hemodynamics, but has had inconsistent results [12]. Direct surgical treatment with bypass of the aneurysmal segment, vessel occlusion thrombectomy and transposition in combination or alone has been described [12]. However, direct surgical intervention is associated with significant morbidity and mortality with 75% of treated patients suffering moderate disability, severe disability, and/or death in a series of 12 patients [15]. Similarly endovascular flow diversion therapies have shown mixed results [12].
No randomized control trials have been performed to investigate surgical interventions; therefore there is no consensus on their effectiveness [7]. Following surgical intervention morbidity risk was 12% and mortality was 20% in a study examining 66 cases of giant fusiform aneurysms of the vertebrobasilar arteries [16]. Therefore, surgical intervention is only recommended in symptomatic patients where outcomes are poor [6].
Primary and secondary prevention of ischemic stroke in patients with VBD is not well defined [17]. However, Pico et al. proposed that if the enlargement of the vertebral artery is ≥2 mm or the basilar artery diameter is ≥10 mm, treatment should be considered. Antiplatelets have been proposed to reduce the risk of ischemic stroke in selected patients, but not those with severely dilated vessels as the risk of hemorrhage may increase [18]. Likewise, a further study suggests that a lack of treatment with anticoagulants in VBD is an independent predictor of all-cause mortality [19]. No evidence-based guidelines exist on the role of anticoagulation or antiplatelet therapy in VBD and therefore treatment is predominantly based on physician opinion [6].
Patient education is important in conditions that carry significant risk of morbidity and mortality. Our patient declined follow-up and monitoring of his condition given the uncertainty surrounding its management. Diagnosing VBD is important to inform patients of the associated risks associated. However, as demonstrated here patients can be left with a sense of helplessness when faced with a diagnosis for which evidence-based treatments are lacking. Therefore, randomized control trials are urgently required to examine the effectiveness of invasive interventions, and provide evidence for secondary prevention of stroke in patients diagnosed with VBD.
Conclusion
Vertebrobasilar dolichoectasia is a rare but plausible cause of isolated cranial nerve symptoms that can present to the otolaryngology clinic. Therefore, it is important for otolaryngologists to be aware of this diagnosis in order to perform appropriate imaging and ensure suitable referrals are made to neurosurgery and stroke medicine.
REFERENCES
1.
McCormack A, Edmondson-Jones M, Somerset S, Hall DA. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res 2016;339:219. [CrossRef]
[Pubmed]

2.
British Tinnitus Association. Number of people living with tinnitus in the UK is set to rise. [Available at: https://www.tinnitus.org.uk/blog/number-of-people]

3.
National Institute for Health and Care Excellence. Tinnitus. [Available at: https://cks.nice.org.uk/tinnitus#!scenario]

4.
Titlic M, Tonkic A, Jukic I, Buca A, Kolic K, Batinic T. Tinnitus caused by vertebrobasilar dolichoectasia. Bratisl Lek Listy 2007;108(10–11):455–7.
[Pubmed]

5.
Gutierrez J, Sacco RL, Wright CB. Dolichoectasia—an evolving arterial disease. Nat Rev Neurol 2011;7(1):41–50. [CrossRef]
[Pubmed]

6.
Wolters FJ, Rinkel GJ, Vergouwen MD. Clinical course and treatment of vertebrobasilar dolichoectasia: A systematic review of the literature. Neurol Res 2013;35(2):131–7. [CrossRef]
[Pubmed]

7.
Pico F, Labreuche J, Amarenco P. Pathophysiology, presentation, prognosis, and management of intracranial arterial dolichoectasia. Lancet Neurol 2015;14(8):833–45. [CrossRef]
[Pubmed]

8.
Passero S, Nuti D. Auditory and vestibular system findings in patients with vertebrobasilar dolichoectasia. Acta Neurol Scand 1996;93(1):50–5. [CrossRef]
[Pubmed]

9.
Huh G, Bae YJ, Woo HJ, Park JH, Koo JW, Song JJ. Vestibulocochlear symptoms caused by vertebrobasilar dolichoectasia. Clin Exp Otorhinolaryngol 2019. [CrossRef]
[Pubmed]

10.
Pico F, Labreuche J, Touboul PJ, Amarenco P; GENIC Investigators. Intracranial arterial dolichoectasia and its relation with atherosclerosis and stroke subtype. Neurology 2003;61(12):1736–42. [CrossRef]
[Pubmed]

11.
Pico F, Labreuche J, Touboul PJ, Leys D, Amarenco P. Intracranial arterial dolichoectasia and small-vessel disease in stroke patients. Ann Neurol 2005;57(4):472–9. [CrossRef]
[Pubmed]

12.
Yuan YJ, Xu K, Luo Q, Yu JL. Research progress on vertebrobasilar dolichoectasia. Int J Med Sci 2014;11(10):1039–48. [CrossRef]
[Pubmed]

13.
Kelly-Hayes M. Influence of age and health behaviors on stroke risk: Lessons from longitudinal studies. J Am Geriatr Soc 2010;58 Suppl 2:S325–8. [CrossRef]
[Pubmed]

14.
Matsumoto K, Yamada K, Hayakawa T. et al. Dolichoectatic basilar artery treated by reducing hemodynamic stress – report of two cases. Neurol Med Chir (Tokyo) 1990;30(9):691–4. [CrossRef]
[Pubmed]

15.
Anson JA, Lawton MT, Spetzler RF. Characteristics and surgical treatment of dolichoectatic and fusiform aneurysms. J Neurosurg 1996;84(2):185–93. [CrossRef]
[Pubmed]

16.
Drake CG, Peerless SJ. Giant fusiform intracranial aneurysms: Review of 120 patients treated surgically from 1965 to 1992. J Neurosurg 1997;87(2):141–62. [CrossRef]
[Pubmed]

17.
Chen Z, Zhang S, Dai Z, et al. Recurrent risk of ischemic stroke due to vertebrobasilar dolichoectasia. BMC Neurol 2019;19(1):163. [CrossRef]
[Pubmed]

18.
Passero SG, Calchetti B, Bartalini S. Intracranial bleeding in patients with vertebrobasilar dolichoectasia. Stroke 2005;36(7):1421–5. [CrossRef]
[Pubmed]

19.
Passero SG, Rossi S. Natural history of vertebrobasilar dolichoectasia. Neurology 2008;70(1):66–72. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jessica Daniels - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Milan Rudic - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2020 Jessica Daniels et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.