|
Clinical Image
Eagle’s syndrome
1 Senior Registrar Otolaryngology, Department of Clinical Surgical Sciences, University of West Indies, Eric Williams Medical Sciences Complex, Champs Fleur, Trinidad and Tobago
2 Otolaryngology Resident, Department of Clinical Surgical Sciences, University of West Indies, Eric Williams Medical Sciences Complex, Champs Fleur, Trinidad and Tobago
3 Consultant Otolaryngologist, Department of Clinical Surgical Sciences, University of West Indies, Eric Williams Medical Sciences Complex, Champs Fleur, Trinidad and Tobago
Address correspondence to:
Nicholas Figaro
Department of Surgery, Eric Williams Medical Sciences Complex, Uriah Butler Highway, Champ Fleurs,
Trinidad and Tobago
Message to Corresponding Author
Article ID: 100006Z18NF2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Figaro N, De Verteuil F, Arozarena R, Juman S. Eagle’s syndrome. J Case Rep Images Otolaryngol 2022;3(2):4–6.ABSTRACT
No Abstract
Keywords: Calcified stylohyoid ligament, Cervicopharyngeal pain, Eagle’s syndrome, Elongated styloid process
Case Report
A 29-year-old male presented to the Otolaryngology Clinic with a three month history of left-sided oropharyngeal odynophagia, otalgia, and retro-orbital pain. The pain was exacerbated by chewing, mouth opening, anteflexion, and rotation of his head to the left and not alleviated by non-steroidal anti-inflammatory drugs (NSAIDs) and anticonvulsants. He had neither a history of trauma, previous surgery nor a significant past medical history.
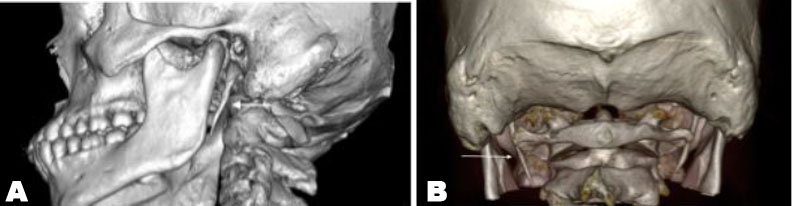
The patient underwent a detailed ear, nose, and throat examination that excluded benign and malignant tumors of the upper aerodigestive tract, temporomandibular joint, and dental pathology. A bony prominence was felt during bimanual palpation of the left tonsillar fossa and severe pain radiating to the ipsilateral ear was evoked during palpation. The contralateral tonsillar fossa was normal. Neurological examination as well as brain and cervical magnetic resonance imaging and angiography were unremarkable. Computed tomography with three-dimensional volume rendering images revealed asymmetric elongation of the stylohyoid processes, which were 37 mm on the left and 31 mm on the right (Figure 1A and Figure 1B). Temporary relief of the patient’s pain was obtained with infiltration of the 1 mL of 2% lidocaine in the left tonsillar fossa.
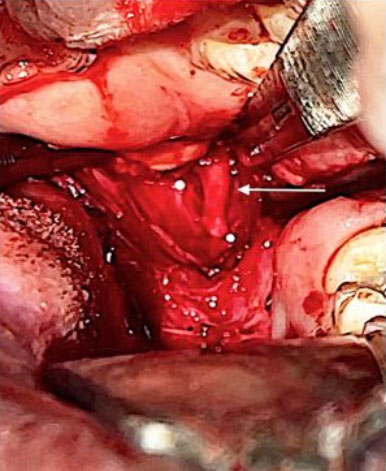
Based on the clinical findings and radiological imaging, the patient was diagnosed with Eagle’s syndrome (ES). Under general anesthesia, via an intraoral approach, the patient had partial surgical removal of the elongated styloid process (Figure 2 and Figure 3). The patient had an uneventful post-operative period and complete resolution of his symptoms.
Discussion
Eagle’s syndrome is a rare condition, clinically characterized by cervicofacial and/or cervicopharyngeal symptoms secondary to an elongated styloid process and/or abnormal calcification of the stylohyoid ligament [1]. The styloid process is widely considered elongated when its length exceeds 30 mm [2]. It is estimated that 4% of the general population possess an elongated styloid process and as such this condition is not unusual. However, only 4–10% of this subset are genuinely symptomatic [3]. The etiology of ES is controversial, as a result several theories have been proposed, namely persistence of embryologic cartilaginous outgrowths and trauma-induced reactive ossification of the styloid process tip or stylohyoid ligament [3],[4].
The stylohyoid complex is in close proximity to several crucial neurovascular structures, specifically the carotid arteries, internal jugular vein, the facial nerve, auriculotemporal nerve, lingual nerve, chorda tympani, glossopharyngeal nerve and hypoglossal nerve. Abnormal elongation of the stylohyoid complex can therefore lead to direct compression of these structures and cause a myriad of symptoms [3],[5]. The patient complaints range from dysphagia/odynophagia, otalgia, foreign body sensation in the pharynx, cervical pain, facial pain, retroorbital pain, auditory symptoms, cluster, and migraine headaches [1],[6].
Due to the vague, non-specific symptoms of ES, it is not surprising that patients may pursue consultations with several clinicians, especially otolaryngologists, neurologists, dental surgeons, and psychiatrists [7]. Consequently, it may be quite challenging to make the diagnosis since a variety of conditions share similar symptomatology and must be excluded. The diagnosis of ES is established on four distinctive parameters: (1) clinical symptoms, (2) manual palpation of the styloid process in the tonsillar fossa, (3) radiological imaging, and (4) lidocaine infiltration test [1],[3].
Therapy for ES may be medical or surgical. A subset of patients will get relief from NSAIDs, anticonvulsants, antidepressants, steroids, and/or local anesthetic infiltration [8].
However, for those patients whose symptoms are refractory to medication, surgical management is advised [1]. The intraoral and external cervical surgical approaches are widely described for the removal of the elongated portion of the styloid process, each with its unique risks and benefits [9]. Despite surgical and non-surgical treatment options for ES, the literature cites a 20% failure rate, which may be due to the multifaceted origin of the condition and the clinical dilemma posed while establishing the root cause of the patient’s symptoms [1],[10].
Conclusion
Eagle’s syndrome has a plethora of clinical presentations as indicated by the wide array of its nonspecific symptoms. Clinicians should be mindful of the existence of such a clinical entity. As a result, ES should be considered in the differential diagnosis of cervicofacial and cervicopharyngeal pain recalcitrant to medical management. A working knowledge of the diagnostic evaluation, radiological imaging, and treatment options of this clinical condition is necessary to mitigate its negative impact on a patient’s quality of life.
REFERENCES
1.
Piagkou M, Anagnostopoulou S, Kouladouros K, Piagkos G. Eagle’s syndrome: A review of the literature. Clin Anat 2009;22(5):545–58. [CrossRef]
[Pubmed]

2.
Asutay F, Erdem NF, Atalay Y, Acar AH, Asutay H. Prevalence of elongated styloid process and Eagle syndrome in east eagean population. Bezmialem Science 2019;7(1):28–32. [CrossRef]

3.
Badhey A, Jategaonkar A, Anglin Kovacs AJ, et al. Eagle syndrome: A comprehensive review. Clin Neurol Neurosurg 2017;159:34–8. [CrossRef]
[Pubmed]

4.
Bouzaïdi K, Daghfous A, Fourati E, Kechaou I, Jabnoun F, Chtioui I. Eagle’s syndrome. Acta Radiol Short Rep 2013;2(5):2047981613495676. [CrossRef]
[Pubmed]

5.
Uludag IF, Öcek L, Zorlu Y, Uludag B. Eagle syndrome: Case report. Agri 2013;25(2):87–9. [CrossRef]
[Pubmed]

6.
Casale M, Rinaldi V, Quattrocchi C, et al. Atypical chronic head and neck pain: Don’t forget Eagle’s syndrome. Eur Rev Med Pharmacol Sci 2008;12(2):131–3.
[Pubmed]

7.
Saccomanno S, Greco F, De Corso E, et al. Eagle’s syndrome, from clinical presentation to diagnosis and surgical treatment: A case report. Acta Otorhinolaryngol Ital 2018;38(2):166–9. [CrossRef]
[Pubmed]

8.
Han MK, Kim DW, Yang JY. Non surgical treatment of Eagle’s syndrome – A case report. Korean J Pain 2013;26(2):169–72. [CrossRef]
[Pubmed]

9.
Mohanty S, Thirumaran NS, Gopinath M, Bambha G, Balakrishnan S. Significance of styloidectomy in Eagle’s syndrome: An analysis. Indian J Otolaryngol Head Neck Surg 2009;61(4):262–5. [CrossRef]
[Pubmed]

10.
Rechtweg JS, Wax MK. Eagle’s syndrome: A review. Am J Otolaryngol 1998;19(5):316–21. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Nicholas Figaro - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Francis De Verteuil - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rodolfo Arozarena - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Solaiman Juman - Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Nicholas Figaro et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.